“ I think the pathways and progress we’ve made for Indigenous youth in Australia has been incredible.
I think there have been more opportunities, there’s more publicity, people are actually aware that there is a pathway for Indigenous youth, not only in tennis but in all sports.
But tennis is now becoming a nationwide sport for Indigenous youth.
It’s incredible to know what Evonne has done and how passionate she is about it. If I can have any small part in that, that would be incredible.”
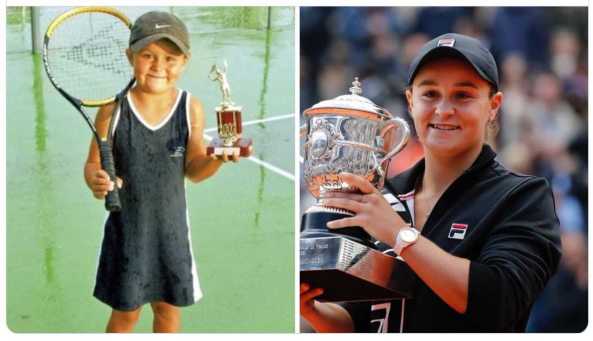
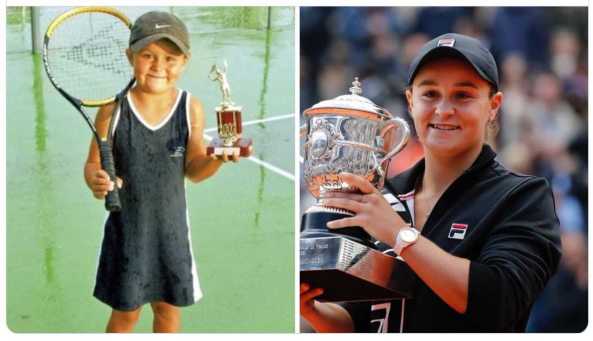
Ash Barty speaking after winning the 2019 French Open 8 June

Her win will inspire a generation of Australian girls to play tennis and as an Indigenous Australian, just like the 1971 champion, Evonne Goolagong Cawley ( 13-time major champion ) See Part 2 and 3 below
” Goolagong grew up in the wheat town of Barrellan in New South Wales, one of eight children. Her mother Melinda was a homemaker and father Kenny a sheepshearer.
Their simple one-story home was a tin shack with dirt floors and no electricity. But moreover, Goolagong was born into Aboriginal heritage, the only family of its kind in town, and as light-skinned members of the Wiradjuri tribe, the Goolagong kids faced prejudice, and faced a cloudy and uncertain future.
The Australian government’s policy at the time was to forcibly remove Aboriginal children from their families and relocate them to camps where they could be properly educated and integrated into white society.
“Every time there was a shiny car, my mum must have worried if was the welfare people coming for her kids,” Goolagong has explained in many media interviews when the topic of her Aboriginal roots was questioned.
“We had no idea. We thought the welfare man was there to take us away.”

Evonne pictured this week with Tackling Tobacco Team – Nunkuwarrin Yunti ACCHO Adelaide
Since 2005, she has run the Goolagong National Development Camp for Indigenous girls and boys, which uses tennis as a vehicle to promote better health, education and employment. See Part 4 below
See Evonne Goolagong Foundation Website
Extracts from the Guardian
Everything you need to know about Ash Barty was summed up in the immediate aftermath of her first grand slam success. Within minutes, the 23-year-old, a teenage prodigy turned cricketer and turned back into a tennis player again, was busy trying to share the glory with those she feels have helped her along the way.
From her family – her parents and her two sisters – to her team, and coach Craig Tyzzer, Barty almost always speaks of “we” when it comes to describing her exploits.

She may be a grand slam champion for the first time, but as far as she is concerned, it has been a team effort.
“I’m extremely lucky to have a team around me that love me for Ash Barty the person, not the tennis player,” she said, sitting with the Coupe de Suzanne Lenglen within reach, just an hour or so after her 6-1, 6-3 triumph over the Czech teenager Markéta Vondroušová.
“I’m extremely lucky to have an amazing family, a truly amazing family that no matter, win lose or draw, the text messages and the facetiming is the same. It’s just a really good group of people around me that make the tennis very easy.”
If it wasn’t already clear, Barty is a hugely popular player, as evidenced by the outpouring of congratulations on social media, and directly to Barty via texts and instant messages.
From Petra Kvitová to Nick Kyrgios and from numerous players and coaches on both the ATP and WTA Tours, Barty’s achievement was hailed by her peers. “It’s incredibly kind, especially from your peers, I suppose,” said Barty, who shared a handshake and hug with Rod Laver after the match.
“And people that you see every single week and most weeks of the year, it’s very kind of them to compliment [me], my game.
But I think it’s also a compliment to my team. It’s just been an incredible journey, the way we have tried to work and develop and grow this game that I have and this game style and kind of Ash Barty brand of tennis, I suppose. It’s amazing. I haven’t seen any of it yet. It’s just been nice to take a minute or two with my team and celebrate what we have achieved.”
There have been some tough days for first-time finalists here at Roland Garros over the years, from Natasha Zvereva being double-bagelled by Steffi Graf in 1988 to Elena Dementieva’s 6-2, 6-2 defeat by Anastasia Myskina in 2004. Barty and Vondroušová were both appearing in their first grand slam final but while the Czech failed to produce her best, Barty was close to perfect in her execution of her game.
And hers is a game to bring a smile to the face of anyone who loves to see variety on the court.
Compete, enjoy and try to do the best you can – that’s her mantra – and the way she plays, with slice, power, angles, drop shots, volleys, kick serves, everything you can imagine, is a joy to watch. As Kirsten Flipkens, the Belgian player, tweeted on Saturday evening: “Just love to watch her play (with a gamestyle similar to mine, just 20 times better. Slice for life! Impressive, Kiddo”.
Three years after she returned from an almost two-year hiatus from the Tour, Barty has a grand slam title to her name, a surprise only in the fact that the first one should come at Roland Garros, rather than, say, Wimbledon, where her style of play would seem to be perfectly suited.

It was at Wimbledon where she won as a junior, aged 15, but her ability to hit every shot, as encouraged by her first coach, Jim Joyce, means she is a threat on every surface.
September 2018 #USOpen Doubles Title

Barty will rise to world No 2 on Monday, only a handful of points behind Naomi Osaka, and she admitted that reaching top spot was a goal.
Barty will celebrate with her family when she heads to the UK for the grass-court season, building to Wimbledon, where she will be a big threat for the title. It’s entirely possible she will be the world No 1 before the summer is out, but whatever success she has, she will ensure her family and team share the credit.

Part 2. Evonne discovers spiritual centre court 1993

When she competed on the world professional tennis circuit Evonne Cawley would always look forward to the traditional dancing that tournament organisers would put on to welcome international players.
But she always wondered why, at the Australian events, no equivalent celebration of Indigenous culture ever took place.
“In almost every other country, I went to the native people would put on a dance,” Cawley recalled this week. “I used to think, “why doesn’t this happen at home ?. It always made me feel a little sad.”
For Cawley, the sporting heroine who as “our girl” Evonne Goolagong rose from the obscurity of small town life in NSW to capture her first Wimbledon crown as a teenager in 1971, such memories are becoming increasingly relevant as she seeks to unravel the mysteries of her own aboriginality.
It is a journey of self-discovery which this week took her, for the first time, to Australia’s red centre, to a dinner with 120 Aboriginal women in Alice Springs and to the awesome grandeur of Uluru, symbolic sentry to 40 000 years of Indigenous Australian culture.
“ I ve reached a stage in my life where I need to find out about where I come from – about everything to do with being an Aboriginal person,”said Cawley.
In the ancient Pitjantjatjara language of the Anangu custodians of Uluru the process is written “ara mulapa ngaranyi pulkara kulintjaku”- the proper thing is to really listen.
As she follows this new road Cawley has found a great source of strength in the old Aboriginal women she has met along way , women she described as the most interesting people I have ever met.”
At dinner in Alice Springs she sat down with traditional Aboriginal women who have never seen a big city, hardly ever left the desert. Gushing with joy, she explained how they held hands together and sang old favourite mission songs like “One Day at a Time”.
“ The dinner was a really special time for me, “Cawley said. “ I had never been to anything like it before and I felt a great sense of unity with the women. I really felt there was a lot of bonding there.”
Cawley’s search for her Aboriginal identity reveals the little-known downside of her life in the jet-set world of professional tennis.
Thrust into the limelight as a teenager by the sheer natural artistry and grace of her sporting talent she inevitably became an international celebrity, feted from nation to nation by the sport’s floating gallery of movie stars, money moguls and royalty.
Front Page The Australian September 11-12 1993
Part 3 Evonne Goolagong 13-time major champion

Evonne Goolagong was not born into tennis royalty with a gold plated racquet, fancy outfits, and private lessons at a posh country club.
From the Tennis Hall of Fame
Furthermore, she didn’t matriculate her game with a used wooden racquet on public courts.
Her introduction to tennis has perhaps the most humble origins in tennis history, yet she overcame major stumbling blocks to become the No. 1 player in the world, won 13 majors and ranked 12th all-time in championship wins.

Goolagong’s first racquet as a youngster was made from a wood fruit box that resembled a paddle – it was absent of any strings. For hours on end she would hit a ball against any flat surface she could find.
A young Evonne was spotted peering through a fence at Barellan War Memorial Tennis Club by club president Bill Kurtzman, who asked her if she’d like to join in. Had Kurtzman not made the gracious and human offer, it’s likely her road to the Hall of Fame, let alone a revered place in history as a two-time Wimbledon Ladies Singles champion (1971, 1980) and keeper of four straight Australian Open Singles titles (1974-77) would not have materialized.
Word obviously traveled fast, as renowned Sydney-based tennis coach Vic Edwards was tipped off to the prodigy and made a 400 mile trip west to the wheat-farming country to see what all the fuss was about.
Even as a developing player, Goolagong had the grace and movement on court that would be a staple of her splendid career. Edwards was enamored with Goolagong, whose name is Aboriginal. He persuaded her parents to let him take the 14-year-old to Sydney for schooling at Willoughby Girls School (where she completed her School Certificate in 1968), coaching, and boarding.
She became part of his family in 1965, with Edwards protecting her from racial slurs, as she competed in big city tournaments, teaching her to believe in herself and talents. Edwards instilled confidence in Goolagong and prepared to her to become the first non-white to play in apartheid South African in a tournament in 1972. At age 15, Goolagong won the New South Wales Championship and in 1967 competed in her first Australian Nationals.
Goolagong would compile an illustrious resume, appearing in 26 major finals (18 singles, six women’s doubles and two mixed doubles), capturing seven singles, five doubles and one mixed double championship.
Overall, she earned 72 singles, 45 doubles and three mixed doubles tour championships and compiled a 704-165 (81 percent) singles record. During the 1970s, Goolagong was a household name and face – attractive, carefree, and admittedly prone to lapses in concentration that caused folks to say “Evonne’s gone walkabout.”
Goolagong was graceful, almost poetic in how beautifully she played the game. Not only did tennis fans marvel in her smooth and effortless movements, but her opponents could also get caught in the ballet that was on the other side of the net.
“She was like a panther compared to me,” said Billie Jean King after losing to Goolagong in the semifinals of the 1974 Virginia Slims Championship at the Los Angeles Sports Arena. “She had more mobility and she played beautifully. I started watching her, and then I’d remember all of a sudden that I had to hit the ball.”
In 2005, Martina Navratilova told Sports Illustrated, “She was such a pretty player. She didn’t serve-and-volley, she would sort of saunter-and-volley.”
Goolagong preferred a baseline game that observers said was reminiscent of Ken Rosewall‘s – her backhand was classically stroked liked Rosewall’s with slice and accuracy. Her groundstrokes were precise and fluid, balls struck hard each time.
“She can be down love-40, apparently beaten, and she’s still trying to hit winners,” Margaret Court told the New York Times. “She won’t play safe tennis, and her shots are quite unpredictable. They’re likely to come back in any direction. The harder you hit the ball to her, the more she likes it. It’s best to slow the game up, rather than try to outbelt her … and she loves a wide ball … she’ll have a crack at anything.”
At the 1971 Australian Open, Goolagong lost to her idol Court in three well-played sets, 2-6, 7-6, 7-5.
At the French Open, the No. 3 seeded Goolagong won her first major singles championship, defeating fellow Aussie and unseeded surprise finalist Helen Gourlay, 6-3, 7-5.
It helped that No. 1 seed Court and No. 2 seed Virginia Wade were eliminated in the third and first rounds respectively. Goolagong didn’t face a seeded player until the quarterfinals, No. 6 Françoise Dürr, and squashed the native favorite, 6-3, 6-0.
A few months later, her tennis dream came true when she decisively defeated Court to win Wimbledon, 6-4, 6-1. “To beat Margaret Court … I was over the moon about winning,” Goolagong said. Outside of defeating the defending champion Court, Goolagong needed a huge semifinal, 6-4, 6-4 victory over King to advance. She nearly became a repeat champion in 1972, but King evened matters with a decisive 6-3, 6-3 victory in the final.
“It was the age of nine that I dreamed about winning Wimbledon,” Goolagong said, appearing as a guest on the television news program Where They Are Now Australia in 2007. “I read this cartoon magazine story called Princess Magazine, about a young girl who was found, trained and taken to this place called Wimbledon, where she played on this magical center court and eventually won. Every time I went to hit against a wall I used to pretend I was there, and every time I went to sleep I would dream about playing on that magical court”
Goolagong made her Wimbledon debut in 1970, and at the time, just stepping inside the hallowed All England Club may have seemed like heaven for the Aussie, but she had unfinished business ahead.
“I remember a cocktail party the night before Wimbledon started and the head of Dunlop (Goolagong’s racquet sponsor) took me out on court when there was no net, just deep silence,” Goolagong recalled. “I said, ‘Wow, I am here … my dream has come true, I am really here.’ I remember playing a girl named Peaches Bartkowitz – what a name – an American top player who beat me pretty convincingly (6-4, 6-0).
When I got off the court my coach said, ‘maybe I better enter you into the “plate” event for second and third round losers, that way you’ll get used to the atmosphere, the crowds, the court. I played in that and ended up winning it.”
The following year, the fairy tale came true with the cherished victory in London and Goolagong ended the 1971 touring season as the Associated Press Female Athlete of the Year.
Wimbledon had a love affair with Goolagong, who dubbed her “Sunshine Supergirl” and she long maintained that the crowning moment in her career came at Wimbledon in 1980, when she defeated Chris Evert in the final to become the first mother since Dorothea Lambert Chambersto accomplish that feat in 1914.
The nine years between championships matched Bill Tilden for the longest gap between titles in history. “After I defeated Margaret Court at Wimbledon in 1971, I found out later she was pregnant and I thought, ‘so that’s why she played so badly,’” Goolagong joked. “Of course I was pregnant in 1980 and was so thrilled to have won again.”
Goolagong captured the Australian Open four times and three consecutively (1974-76), defeating Evert (7-6, 4-6, 6-0); Navratilova (6-3, 6-2) and Czech Renata Tomanova (6-2, 6-2).
The three-peat at Melbourne has only been accomplished by Court, Steffi Graf, Monica Seles, and Martina Hingis. Goolagong also appeared in six consecutive finals (1971-77), a record shared with Hingis and stands alone in total finals (7), achieved from 1971-76. Three of her wins (1975-77) came without losing a set, a remarkable mark shared only with Graf. The only asterisk on her championship-filled career was the U.S. Open, where she was a finalist four consecutive times (1973-76), and unable to claim a championship, though the 1973, 1974, and 1975 defeats all came in tightly-contested three set matches against Court, King, and Evert.
Goolagong was nearly perfect in doubles, winning seven major tournaments; 1971 Australian with Court, 1974 Australian and Wimbledon alongside American Peggy Michell; 1975 Australian with Michell; 1976 and 1977 Australian with compatriot Helen Gourlay. She won the 1972 French Open Mixed Doubles Championship with Aussie partner Kim Warwick.
Goolagong made history in October, 1974. As a 23-year-old, she won the third annual and season-ending Virginia Slims Championship played at the Los Angeles Sports Arena. She upset King in the semifinals, 6-2, 4-6, 6-3 and then upset Chris Evert in the final, 6-3, 6-4. She earned $32,000, equal to the top cash prize in the history of women’s tennis. Goolagong also won the season-ending Slims in 1976, again defeating Evert. She was a finalist in 1978, losing to Martina Navratilova. She ranked in the Top 10 for nine years. She married Roger Cawley in 1975 and added the surname while still on tour.
Nagging injuries forced her into retirement in 1983. She moved to South Carolina, where she became the touring professional at the Hilton Head Racquet Club. The family purchased 70 acres and built a 20-court tennis center. She began working with Tennis Australia and launched the Evonne Goolagong Getting Started program for young girls.
For her service to tennis, Goolagong was appointed Member of the Order of the British Empire in 1972 and Officer of the Order of Australia in 1982. Home! The Evonne Goolagong Story was published in 1993. Since 2005, she has run the Goolagong National Development Camp for Indigenous girls and boys, which uses tennis as a vehicle to promote better health, education and employment.
Part 4

Part 4 ABOUT THE EVONNE GOOLAGONG FOUNDATION PROGRAMS
DREAM – BELIEVE – LEARN – ACHIEVE!
Under the auspices of the Evonne Goolagong Foundation, the Goolagong National Development Camp targets Indigenous young people between the ages of 12 and 21 for four main purposes:
- Use tennis as a vehicle to promote and help provide high quality education and teach better health through diet and exercise.
- Increase the number of young Indigenous people playing tennis both competitively and socially
- Support young Indigenous people who have the potential to play at the elite level and make a career in tennis either as a player, coach or administrator.
- Develop in all young people who come through the camps the ability to lead, plan and organise so they can contribute these skills in their own Communities when they return as well as work effectively with non-Indigenous individuals and organisations.
See Evonne Goolagong Foundation Website
Since 2012, in partnership with the Australian Government the Dream, Believe, Learn, Achieve programme each year has run ‘Come and Try’ days across each State and Territory with some participants chosen to receive assisted coaching.

Progression to a Goolagong State Development Camp (GSDC) can follow with the aim of selection to the Goolagong National Development Camp (GNDC) held each January in Melbourne during the first week of the Australian Open.
Mentored school scholarships are awarded from the GNDC. To date, almost 4900 youngsters have entered the programme and in 2017 thirty youngsters have progressed to the GNDC 2018.

Like this:
Like Loading...